Have you ever wondered what it feels like to be on a ventilator? If you or a loved one ever face this situation, you might ask: Can you be conscious while on a ventilator?
Understanding this can ease your fears and help you prepare for what lies ahead. You’ll discover the truth about awareness during ventilation, what to expect, and how medical teams keep you safe. Keep reading to get clear answers that matter to you.
Consciousness And Ventilation
Understanding consciousness while on a ventilator can be confusing. Many people wonder if a person can truly be aware when machines assist their breathing. The truth depends on how the ventilator works and the level of sedation used during treatment.
How Ventilators Work
A ventilator is a machine that helps you breathe when your lungs cannot do it effectively on their own. It pushes air, often with extra oxygen, into your lungs through a tube inserted in your windpipe or nose.
The machine controls the rhythm, volume, and pressure of each breath. This support can range from partial help to full control of breathing. Because it handles the work of your lungs, your body gets the oxygen it needs to function.
But being on a ventilator doesn’t automatically mean you lose consciousness. The machine’s role is to assist breathing, not to put you to sleep.
Sedation And Awareness Levels
Doctors often use sedation to keep patients comfortable on a ventilator. Sedation reduces anxiety and prevents discomfort caused by the breathing tube. However, the depth of sedation varies based on the patient’s condition.
Some patients remain fully awake and aware while on ventilators. Others might be lightly sedated but still able to respond to voices or touch. Deep sedation or anesthesia is sometimes necessary for severe cases or during surgery, which leads to unconsciousness.
Have you ever thought about what it feels like to be awake but unable to speak or move because of a breathing tube? Many patients describe mixed emotions—fear, confusion, but also moments of clarity and hope.
Understanding these differences can help you better communicate with healthcare providers or support a loved one on a ventilator. It’s important to ask about sedation plans and express your comfort needs clearly.
Credit: ccforum.biomedcentral.com
Experiences Of Patients On Ventilators
Being on a ventilator is often seen as a state where patients are unconscious or heavily sedated. However, many patients share surprising stories about their experiences while connected to these machines. Their accounts reveal a complex blend of awareness, sensation, and memory that challenges common assumptions.
Cases Of Awareness
Some patients report moments of clear consciousness despite being on a ventilator. They recall conversations, sounds, and even feelings of panic or calm during their treatment. These instances highlight that sedation doesn’t always guarantee complete unconsciousness.
One patient described hearing doctors discussing their condition and feeling helpless but fully aware. Another remembered the sensation of the breathing tube and the struggle to communicate. These experiences raise important questions about how medical teams monitor patient awareness and comfort.
Common Sensations And Memories
Many patients describe physical sensations that stand out during their time on a ventilator. Dry mouth, pressure from the tube, and difficulty swallowing are frequent complaints. These sensations often leave a lasting impression, even after recovery.
Memory of fear or confusion is also common. Patients may feel trapped or isolated, unable to express themselves. Understanding these feelings can help you or your loved one prepare mentally and emotionally if ventilator support becomes necessary.
- Patients often remember the noise of the machine and alarms.
- Some report dreams or hallucinations linked to medication.
- Feeling cold or shivering despite blankets is common.
How would you cope knowing you might be aware but unable to move or speak? These personal experiences emphasize the need for compassionate care and careful sedation management.
Factors Influencing Consciousness
Understanding what affects consciousness while on a ventilator can clarify many concerns you or your loved ones might have. Consciousness doesn’t just depend on the machine itself but on a mix of medical and technical factors. Let’s look at what truly influences whether someone stays aware or drifts into unconsciousness during ventilator use.
Sedative Medications
Sedatives are often given to make ventilator use more comfortable and to prevent anxiety or pain. These medications directly impact your brain’s alertness by slowing down nerve activity.
The type and dose of sedatives can change how awake or drowsy you feel. Some people might need just a light touch, while others require deeper sedation to tolerate the breathing tube.
Have you ever noticed how even a small dose of medicine can make you sleepy? In critical care, finding the right balance is crucial to keep you calm but still conscious enough to respond.
Medical Conditions
Your overall health plays a big role in consciousness during ventilation. Conditions like brain injury, infections, or severe lung disease can lower your awareness independently of medication.
For example, if your brain is swollen or not getting enough oxygen, you might be unconscious regardless of the ventilator settings.
Think about how a fever or severe illness can make you feel confused or sleepy. In intensive care, these factors are carefully monitored to understand their impact on your consciousness.
Ventilator Settings
The machine itself can influence how awake you feel. Settings that control oxygen levels, breathing rate, and pressure affect your comfort and brain oxygen supply.
If the ventilator is set too aggressively, it might cause discomfort or even harm, leading your body to shut down consciousness as a protective response.
Conversely, if the settings are too low, your body may struggle to get enough oxygen, also affecting alertness. Adjustments happen constantly to match your needs.
Credit: www.theglobeandmail.com
Risks Of Being Conscious On A Ventilator
Being conscious while on a ventilator presents unique challenges that go beyond the physical need for breathing support. It’s not just about staying alive; it’s about how your mind and body respond to the experience. Understanding the risks involved can help you prepare mentally and physically if you or a loved one faces this situation.
Psychological Impact
Staying awake on a ventilator can trigger intense feelings of anxiety and fear. You may feel trapped, unable to speak, or worry about your health worsening. Some patients report vivid nightmares or hallucinations, making the experience even more distressing.
Have you ever felt panic when you couldn’t catch your breath? Imagine that feeling multiplied, with no way to control it. This stress can affect your recovery and overall mental health.
Physical Discomfort
The physical sensation of the ventilator tube can cause irritation in your throat and mouth. This discomfort can make swallowing difficult and increase saliva production, which might lead to coughing or choking sensations.
Muscle weakness is another concern. Because the ventilator does much of the breathing work, your breathing muscles can become weak, making it harder to breathe on your own once the ventilator is removed.
Communication Challenges
Being conscious but unable to speak is one of the most frustrating aspects of ventilator use. Traditional speech isn’t possible with a breathing tube in place, leaving you with limited ways to express pain, fear, or basic needs.
Many patients rely on eye movements, hand signals, or communication boards. However, these methods can feel slow and inadequate, increasing feelings of isolation. How would you cope if you couldn’t easily tell someone you’re uncomfortable or scared?
Improving Patient Experience
Patients on ventilators can sometimes stay awake and aware during treatment. Understanding this helps improve comfort and care during their hospital stay. Clear communication supports a better patient experience.
Improving the patient experience on a ventilator is crucial. Many people wonder if one can be conscious while on this life-support machine. The experience can be unsettling. But, with the right measures, it can be more comfortable.Sedation Protocols
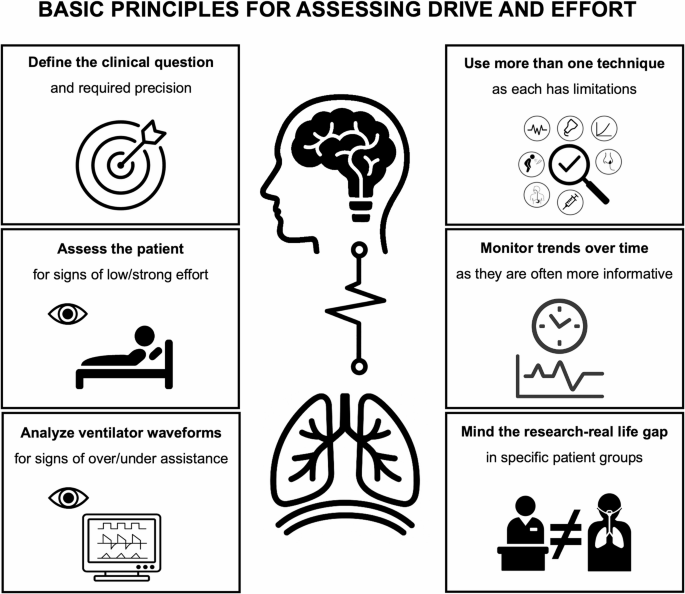
Sedation is key in managing a patient’s comfort on a ventilator. Health professionals use specific protocols to decide sedation levels. The goal? Keep the patient comfortable yet aware. Some patients may need light sedation. Others might require deeper sedation. It’s all about balance. Sedation helps reduce anxiety and discomfort.Monitoring Awareness
Monitoring a patient’s awareness is crucial. Regular checks ensure that the patient is neither over-sedated nor in distress. Tools and observation help in assessing awareness. Nurses and doctors look for signs of consciousness. Eye movement, facial expressions, and body gestures are indicators. These observations guide necessary adjustments.Supportive Care Measures
Supportive care measures enhance the patient’s experience. Simple actions make a big difference. Frequent communication is vital. Reassuring words can calm anxious patients. Playing soft music or offering familiar smells can be comforting. Family visits, when possible, provide emotional support. Ensuring a calm environment aids recovery. Patients on ventilators face a challenging time. But, with thoughtful care, their experience can improve significantly.Future Directions In Ventilator Care
The future of ventilator care is moving toward more precise and compassionate treatment. Advances aim to improve patient comfort and awareness during ventilation. New technologies and approaches may help patients stay more conscious and connected while receiving breathing support.
These developments focus on better monitoring, tailored sedation, and patient-centered care. Each step helps reduce confusion and improve recovery chances. Here are some key directions shaping the future of ventilator care.
Advanced Monitoring Technologies
New sensors and devices track brain activity and vital signs continuously. This data helps doctors understand how awake or sedated a patient is. Real-time feedback allows quicker adjustments to ventilator settings. It also helps detect signs of discomfort or distress early.
Non-invasive brain monitoring tools are becoming more common. They offer insights without causing extra harm or discomfort. These tools support safer and more aware ventilation management.
Personalized Sedation
Tailoring sedation to each patient’s needs is a major focus. Doctors use detailed data to find the right drug type and dose. The goal is to keep patients calm but conscious enough to respond. Personalized sedation reduces risks of over-sedation or delirium.
New protocols aim to balance comfort and awareness carefully. Adjustments happen based on patient feedback and monitoring results. This makes ventilation less stressful and more humane.
Patient-centered Approaches
Care plans now emphasize the patient’s experience and involvement. Patients may participate in decisions about their sedation and ventilation. Communication tools help patients express discomfort or needs even while ventilated.
Family involvement and emotional support are part of this approach. It creates a more supportive environment for recovery. Patient-centered care improves mental health and overall outcomes.

Credit: medium.com
Frequently Asked Questions
Can Patients Be Fully Conscious On A Ventilator?
Yes, many patients remain fully conscious while on a ventilator. Consciousness depends on sedation levels and underlying conditions.
How Does A Ventilator Affect Brain Awareness?
A ventilator supports breathing but does not directly impact brain awareness. Sedatives given during ventilation can alter consciousness.
Can Anxiety Occur While Being Ventilated?
Yes, patients can experience anxiety on a ventilator due to discomfort or fear. Proper care and communication help ease anxiety.
Is It Possible To Communicate While On A Ventilator?
Communication is possible using non-verbal methods like writing or gestures. Some patients may use speaking valves if able to talk.
Conclusion
Being on a ventilator does not always mean losing consciousness. Many patients stay awake and aware while using one. Doctors carefully monitor and adjust settings to keep patients comfortable. Feeling calm and safe matters a lot during this time. Understanding this helps reduce fear and confusion.
Each person’s experience is different and depends on their health. Staying informed can make a big difference in how you cope. Ventilators support breathing but do not control the mind. Awareness can remain even in serious medical situations.





