Have you ever wondered what happens when ventilation during Advanced Cardiac Life Support (ACLS) goes beyond the recommended limits? Excessive ventilation might seem like a good idea when trying to save a life, but it can actually cause serious problems.
Understanding these effects is crucial, especially if you are a healthcare provider or someone interested in emergency care. You’ll discover why too much ventilation can harm the patient and what you can do to avoid common mistakes. Keep reading to learn how to make every breath count during ACLS and improve outcomes when every second matters.
Basics Of Ventilation Acls
Ventilation ACLs are rules used to control airflow in a network. They help manage how data moves through systems and secure sensitive parts. Understanding the basics of ventilation ACLs is key to knowing their impact, especially when applied excessively.
Purpose And Function
Ventilation ACLs control access to network resources. They allow or block traffic based on set rules. Their main goal is to protect networks from unauthorized use. By filtering data packets, they maintain network integrity and performance.
These ACLs act as gatekeepers, deciding which data can pass. They work by examining information like source and destination addresses. This helps prevent unwanted or harmful traffic from entering the network.
Common Usage Scenarios
Ventilation ACLs are common in many network setups. They secure office networks by limiting access to certain systems. They also manage traffic in cloud environments, ensuring safety and efficiency.
Network administrators use these ACLs to:
- Block untrusted devices from accessing sensitive data.
- Control bandwidth by restricting certain traffic types.
- Enhance security by limiting exposure to external threats.
- Segment networks to separate different user groups.
Proper use helps networks run smoothly and safely. Excessive ventilation ACLs, however, can cause issues by over-restricting traffic.
Causes Of Excessive Ventilation
Excessive ventilation during ACLS can cause serious issues. Understanding the causes helps prevent these problems. It involves several factors, including equipment, human error, and the environment.
Equipment Malfunction
Faulty ventilators or monitors can deliver wrong air volumes. Malfunctioning equipment may cause too much or too little ventilation. Regular checks and maintenance reduce this risk.
Operator Errors
Improper training or stress can lead to mistakes. Operators might give breaths too fast or too hard. Clear protocols and practice help avoid these errors.
Environmental Factors
Noise, poor lighting, and distractions affect focus. Crowded or chaotic scenes can increase ventilation mistakes. A calm and organized setting improves performance.
Physiological Impact On Patients
Excessive ventilation during advanced cardiac life support (ACLS) can cause serious harm to patients. The body’s delicate balance is disturbed, leading to several physiological problems. Understanding these impacts helps healthcare providers avoid complications and improve patient outcomes.
Lung Injury Risks
Too much ventilation pressure can damage lung tissues. Over-inflation stretches the alveoli, causing air leaks or rupture. This may lead to pneumothorax or lung collapse. The risk of inflammation and infection also rises. Protecting the lungs means controlling ventilation volume and rate carefully.
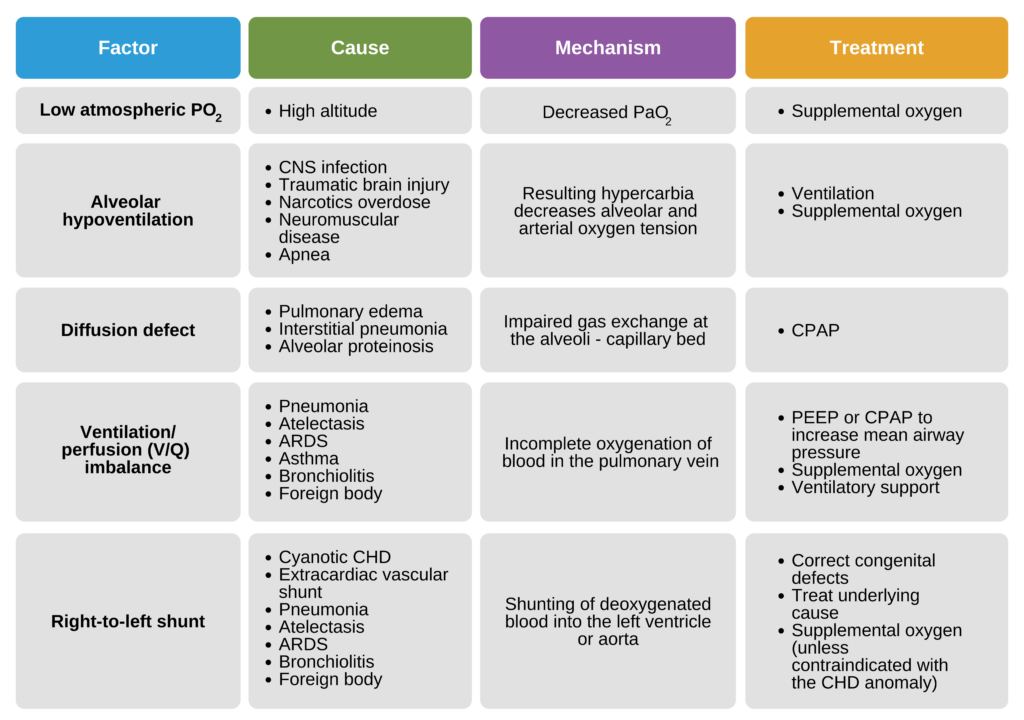
Blood Gas Imbalance
Excessive ventilation changes the levels of oxygen and carbon dioxide in the blood. Too much air removes carbon dioxide too quickly, causing low carbon dioxide levels (hypocapnia). This disrupts the blood’s acid-base balance. The result can be dizziness, muscle cramps, or worse. Maintaining normal blood gas levels is crucial for brain and organ function.
Cardiovascular Effects
Over-ventilation impacts the heart and blood circulation. High pressure in the chest reduces blood flow back to the heart. This lowers the heart’s output and blood pressure. The brain and organs may receive less oxygen-rich blood. Careful ventilation helps keep the heart stable and supports overall circulation.
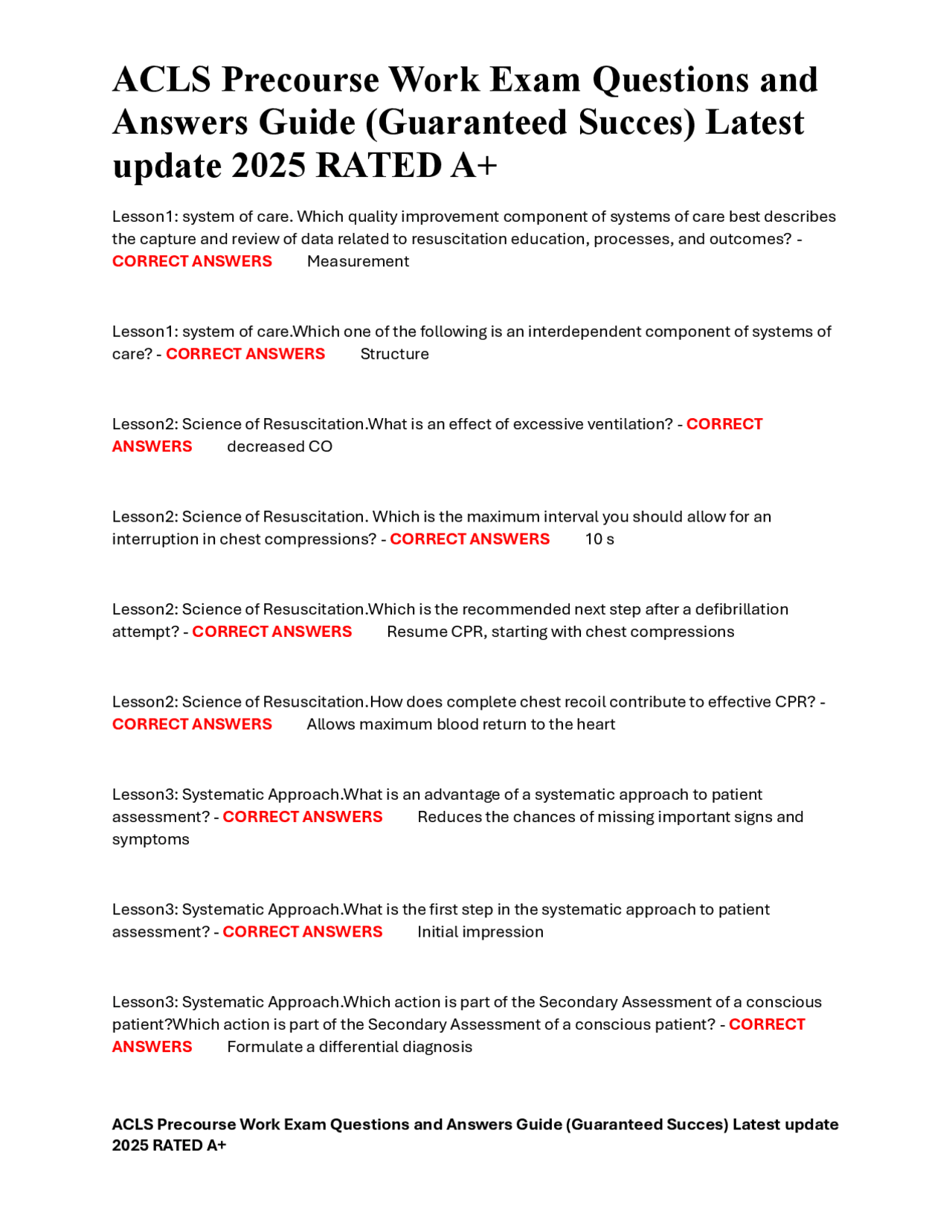
Credit: www.docsity.com
Technical And Operational Risks
Excessive ventilation ACLs can introduce several technical and operational risks that impact both the efficiency and safety of your system. These risks often go unnoticed until they cause significant disruptions, making it essential to understand their effects clearly. Addressing these challenges early can save you time, money, and avoid potential hazards.
Device Wear And Tear
Continuous overuse of ventilation ACLs accelerates device wear and tear. Mechanical parts may degrade faster, leading to frequent breakdowns and costly repairs. Have you ever noticed your equipment needing maintenance more often after heavy use? This is a direct result of pushing devices beyond their intended limits.
Regular monitoring can help detect early signs of damage. Implementing a maintenance schedule based on actual usage rather than time alone can extend device lifespan. Don’t wait for a failure to act—proactive care prevents unexpected downtime.
System Overload
Excessive ventilation can cause your system to overload, affecting overall performance. Overloaded systems slow down, creating bottlenecks and reducing the quality of air management. This can also increase energy consumption, which hikes up operational costs.
Think about the last time your system struggled to keep up with demand. Was it due to too many ACLs running simultaneously? Balancing ventilation loads and optimizing system capacity can maintain smooth operation and prevent costly interruptions.
Alarm Fatigue
Too many ventilation ACLs often generate excessive alarms, leading to alarm fatigue. When alarms sound too frequently, you may start ignoring them, increasing the risk of missing critical warnings. This is a dangerous scenario, especially in environments where safety depends on timely responses.
To combat alarm fatigue, customize alarm settings to prioritize urgent alerts and reduce false positives. Training your team to recognize and respond appropriately can improve safety and operational efficiency. How often do you find yourself dismissing alarms that seem irrelevant? Adjusting your system can change that.
Preventive Strategies
Excessive ventilation during ACLS can lead to reduced blood circulation and increased risk of lung injury. Preventive strategies include monitoring ventilation rates and using appropriate airway management techniques to maintain optimal patient outcomes.
Excessive ventilation during ACLS (Advanced Cardiovascular Life Support) can have serious repercussions, ranging from decreased cardiac output to increased intrathoracic pressure. To mitigate these risks, adopting preventive strategies is crucial. These strategies ensure that ventilation is effective and safe, promoting better patient outcomes.Proper Training
Proper training is paramount in preventing excessive ventilation. Ensure that every member of your medical team is well-versed in the latest ACLS guidelines. Regular workshops and simulations can boost confidence and competence, allowing for swift and precise action during emergencies. Consider incorporating real-life scenarios into training sessions. This approach helps prepare your team for high-pressure situations. Remember, consistency in training translates to consistency in care.Regular Maintenance
Regular maintenance of ventilation equipment is another key preventive strategy. Equipment that is not functioning optimally can lead to inaccurate ventilation rates and volumes. Routine checks and servicing help maintain the accuracy and efficiency of the equipment. Create a checklist for daily and weekly equipment inspections. This proactive approach can prevent unexpected malfunctions. Always have a backup plan for equipment failure to ensure uninterrupted patient care.Monitoring Protocols
Implementing robust monitoring protocols is essential for preventing excessive ventilation. Use capnography and other monitoring tools to keep track of ventilation rates. These tools provide real-time feedback, allowing for immediate adjustments when necessary. Establish clear guidelines on how to respond to deviations in monitored parameters. Engage your team in developing these protocols to ensure they are comprehensive and easy to follow. Are you confident that your current monitoring practices are up to standard? By focusing on these preventive strategies, you can significantly reduce the likelihood of excessive ventilation in ACLS. Prioritize training, maintenance, and monitoring to enhance patient safety and care quality.Case Studies Of Critical Incidents
Examining case studies of critical incidents helps us understand the effects of excessive ventilation during Advanced Cardiac Life Support (ACLS). These real events show how too much ventilation can harm patients. They reveal mistakes made and outcomes faced by medical teams.
By studying these incidents, healthcare workers learn safer ways to manage ventilation. It highlights the importance of proper training and adherence to guidelines. Insights from these cases improve patient care and reduce risks in emergencies.
Real-world Examples
- A patient received rapid, high-volume breaths during resuscitation.
- Excessive ventilation caused increased chest pressure, lowering blood flow.
- This led to reduced oxygen delivery and worsened heart function.
- Another case showed gastric inflation from too much air in the stomach.
- Gastric inflation caused vomiting and airway blockage, risking choking.
- A team failed to monitor ventilation rate, causing dangerous carbon dioxide loss.
- All cases ended with longer recovery times and more complications.
Lessons Learned
- Ventilation rates must match recommended guidelines to prevent harm.
- Medical teams need training to recognize signs of over-ventilation.
- Use of feedback devices helps control breath volume and rate.
- Constant monitoring during ACLS is crucial to adjust ventilation quickly.
- Clear communication among team members prevents ventilation errors.
- Understanding risks leads to safer and more effective resuscitation.
Future Trends In Ventilation Safety
The future of ventilation safety is rapidly evolving to address the challenges posed by excessive ventilation ACLs. Advances in technology and smarter monitoring systems are transforming how risks are detected and managed. This progress aims to protect both equipment and personnel more effectively than ever before.
Technological Innovations
New technologies are making ventilation systems smarter and safer. Automated controls can adjust airflow in real-time, preventing excessive ventilation before it causes harm. Imagine a system that learns from past incidents and adapts to avoid repeating the same mistakes.
Materials used in ventilation equipment are also improving, becoming more durable and resistant to damage from overuse. This means less downtime and fewer costly repairs. Are you ready to trust machines that think ahead and keep your environment safe?
Improved Monitoring Tools
Monitoring tools are becoming more precise and easier to use. Sensors now track airflow, pressure, and air quality continuously, sending alerts the moment something goes wrong. This allows for faster responses and reduces the risk of accidents.
Data analytics play a big role by identifying patterns that humans might miss. For example, detecting subtle changes in ventilation that hint at future problems. Could better data help you prevent issues before they even start?
Credit: aclscertification.org

Credit: heartstartcpr.net
Frequently Asked Questions
What Happens During Excessive Ventilation In Acls?
Excessive ventilation in ACLS causes increased intrathoracic pressure. This reduces venous return to the heart, lowering cardiac output and blood flow to vital organs. It may also lead to gastric inflation and decreased oxygen delivery, worsening patient outcomes during resuscitation.
Why Is Excessive Ventilation Harmful In Cardiac Arrest?
Excessive ventilation during cardiac arrest decreases heart efficiency and blood circulation. It increases intrathoracic pressure, reducing blood flow to the brain and heart. This can worsen hypoxia and reduce the chances of successful resuscitation and survival.
How Does Excessive Ventilation Affect Patient Outcomes?
Excessive ventilation negatively impacts patient outcomes by lowering cardiac output and oxygen delivery. It increases complications like lung injury and gastric inflation. Proper ventilation rates improve oxygenation and enhance the chances of recovery during ACLS.
What Is The Recommended Ventilation Rate In Acls?
The recommended ventilation rate during ACLS is 10 breaths per minute for adults. This rate balances oxygen delivery while preventing excessive intrathoracic pressure. Following guidelines helps optimize patient outcomes during resuscitation efforts.
Conclusion
Excessive ventilation during ACLs can cause serious problems. It may lower carbon dioxide too much, leading to dizziness and poor blood flow. The heart and brain might not get enough oxygen. It can also increase pressure in the chest, making it harder to breathe.
Keeping ventilation at the right level is very important. Careful monitoring helps avoid these risks. Proper ventilation supports better patient recovery and safety. Always balance oxygen and carbon dioxide during ACLs for best results. Simple steps make a big difference in care quality.