Are you curious about how your lungs actually work when you breathe? Understanding how to calculate alveolar ventilation can unlock important insights into your respiratory health.
This simple yet powerful concept shows you how much fresh air reaches the part of your lungs where oxygen enters your blood. By learning this calculation, you’ll gain a clearer picture of how efficiently your body is getting the oxygen it needs.
Keep reading, and you’ll discover easy steps to measure alveolar ventilation and why it matters for your overall well-being.
Basics Of Alveolar Ventilation
Understanding the basics of alveolar ventilation is key to grasping how breathing supports the body’s oxygen needs. Alveolar ventilation measures the amount of air reaching the lungs’ alveoli, where gas exchange happens. This process directly affects oxygen delivery to the blood and removal of carbon dioxide.
Alveolar ventilation differs from total lung ventilation because it excludes air in the dead space. Dead space is the part of the respiratory system where no gas exchange occurs, like the trachea and bronchi. Focusing on alveolar ventilation helps assess effective breathing and lung function.
Definition And Importance
Alveolar ventilation is the volume of air per minute that reaches the alveoli for gas exchange. It is vital for maintaining the right oxygen and carbon dioxide levels in the blood. Poor alveolar ventilation can lead to low oxygen and high carbon dioxide in the body.
Doctors use alveolar ventilation to evaluate lung health and diagnose respiratory conditions. It also guides treatment for patients with breathing difficulties or lung diseases.
Role In Respiratory Physiology
Alveolar ventilation controls how well oxygen enters the blood and carbon dioxide leaves it. It balances the gases during each breath cycle, supporting cell function throughout the body.
This process works closely with the heart and blood vessels. Oxygen-rich blood travels from the lungs to the heart, then pumps to all body parts. Carbon dioxide returns to the lungs to be exhaled.
The efficiency of alveolar ventilation depends on breathing rate, depth, and dead space volume. Changes in any of these affect gas exchange and overall respiratory health.

Credit: www.youtube.com
Key Components To Measure
Calculating alveolar ventilation requires understanding certain key components. These components help measure the amount of air reaching the lungs’ gas exchange areas. Each part plays a vital role in determining how effectively the lungs provide oxygen to the blood.
Accurate measurement of these elements ensures better analysis of lung function. Knowing these values helps in assessing respiratory health clearly and simply.
Tidal Volume
Tidal volume is the amount of air inhaled or exhaled in a normal breath. It usually ranges between 400 to 600 milliliters in adults. This volume represents the air moving in and out during quiet breathing. It is important to measure tidal volume to estimate how much air reaches the lungs with each breath.
Dead Space Volume
Dead space volume is the part of the air that does not participate in gas exchange. This air stays in the airways like the nose, throat, and bronchi. It usually accounts for about 150 milliliters in adults. Measuring dead space helps to subtract the air that does not reach the alveoli from the total breath volume.
Respiratory Rate
Respiratory rate is the number of breaths taken per minute. It varies based on activity, age, and health. A normal resting rate is between 12 and 20 breaths per minute. Counting breaths accurately is essential to calculate total ventilation over time.
Step-by-step Calculation
Calculating alveolar ventilation helps you understand how much fresh air actually reaches your lungs for gas exchange. It’s a practical skill, especially if you’re studying respiratory physiology or monitoring ventilation in clinical settings. Let’s break down the process so you can calculate it confidently.
Subtracting Dead Space
First, you need to find the volume of air that doesn’t participate in gas exchange, known as dead space. This includes air in your trachea and bronchi that never reaches the alveoli.
To calculate, subtract the dead space volume from the total tidal volume (the amount of air you breathe in with each breath). For example, if your tidal volume is 500 mL and your dead space is 150 mL, the calculation is:
- Alveolar volume per breath= Tidal volume – Dead space volume
- 500 mL – 150 mL = 350 mL
This 350 mL represents the air available for gas exchange in each breath. Have you ever noticed how shallow breathing feels less effective? That’s often because dead space takes up a bigger proportion of each breath.
Multiplying By Respiratory Rate
Next, multiply the alveolar volume per breath by your respiratory rate—the number of breaths you take per minute. This step tells you the total volume of fresh air reaching the alveoli every minute.
If your respiratory rate is 12 breaths per minute, continuing with the previous example:
- Alveolar ventilation per minute= Alveolar volume per breath × Respiratory rate
- 350 mL × 12 = 4200 mL/min (or 4.2 L/min)
This means 4.2 liters of air reach your alveoli each minute for oxygen and carbon dioxide exchange. How might this number change if you start exercising or feel stressed? Understanding this helps you see how your body adapts to different demands.

Credit: quizlet.com
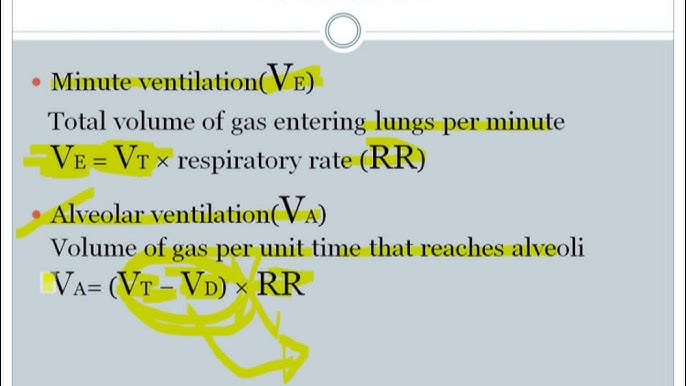
Common Formulas Used
Calculating alveolar ventilation helps understand how much air reaches the lungs for gas exchange. Several formulas exist to measure this vital function. These formulas consider different factors such as breath rate, tidal volume, and dead space. Using the right formula improves accuracy in both research and clinical practice.
Standard Alveolar Ventilation Equation
The standard formula calculates alveolar ventilation by removing dead space from tidal volume. It looks like this:
- Alveolar Ventilation (VA) = (Tidal Volume – Dead Space) × Respiratory Rate
Tidal volume is the air moved in one breath. Dead space is the air that does not reach the alveoli. Respiratory rate is the number of breaths per minute. This formula gives the volume of fresh air reaching the alveoli each minute.
Adjustments For Clinical Settings
Clinical conditions can affect the accuracy of the standard formula. Adjustments may include:
- Using estimated or measured dead space values based on patient condition
- Accounting for changes in respiratory rate due to illness or medication
- Incorporating partial pressure of carbon dioxide (PaCO2) for precise ventilation assessment
These adjustments help tailor calculations to individual patients. They improve the monitoring of lung function in hospitals and clinics.
Factors Affecting Accuracy
Accuracy depends on factors like correct measurement of tidal volume and dead space. Breathing patterns and equipment precision also affect alveolar ventilation calculations. Understanding these helps improve reliable results.
Calculating alveolar ventilation is essential for understanding lung function. Its accuracy can be influenced by various factors. These factors can significantly alter the results. Understanding them helps improve measurement precision.Variations In Dead Space
Dead space refers to areas in the respiratory system where no gas exchange occurs. This includes the trachea and bronchi. Variations in dead space can impact ventilation calculations. For example, a larger dead space reduces effective alveolar ventilation. Conditions like chronic obstructive pulmonary disease (COPD) can increase dead space. Accurate measurement requires considering these variations. Ignoring them leads to incorrect results.Changes In Breathing Patterns
Breathing patterns can vary due to many reasons. Stress, exercise, and illness are common factors. Rapid shallow breathing reduces alveolar ventilation efficiency. Slow deep breathing increases it. Changes in patterns affect the volume of air reaching alveoli. Monitoring these patterns is crucial. It ensures a more accurate calculation of alveolar ventilation. Understanding these changes helps in better health assessments.Practical Applications
Understanding how to calculate alveolar ventilation is more than just a theoretical exercise—it has real impact on patient care and treatment decisions. Knowing the practical uses helps you see why this calculation matters beyond textbooks. It allows you to assess how well a patient’s lungs are functioning in everyday clinical scenarios.
Monitoring Patient Ventilation
Alveolar ventilation gives a clear picture of the air actually reaching the gas exchange areas of the lungs. This measurement helps you track how effectively a patient is breathing, especially those on mechanical ventilation. You can adjust ventilator settings based on this data to ensure the patient gets enough oxygen without causing lung damage.
In critical care, small changes in alveolar ventilation can signal worsening respiratory status before obvious symptoms appear. This early warning system lets you intervene sooner. Have you ever noticed a patient’s sudden drop in oxygen levels? Calculating alveolar ventilation might have helped predict that change.
Assessing Respiratory Disorders
Alveolar ventilation also plays a key role in diagnosing and managing respiratory diseases like COPD or asthma. By comparing alveolar ventilation to normal values, you can pinpoint ventilation problems caused by airway obstruction or lung tissue damage. This helps you tailor treatments more precisely.
For example, a patient with reduced alveolar ventilation despite normal breathing rate could have increased dead space ventilation. This insight changes the way you approach therapy, focusing on improving alveolar air flow rather than just increasing respiratory rate. What patterns in ventilation might you be missing in your patients?

Credit: www.osmosis.org
Frequently Asked Questions
What Is Alveolar Ventilation In Simple Terms?
Alveolar ventilation is the amount of air reaching the lung alveoli for gas exchange. It excludes dead space air that doesn’t participate in gas exchange, ensuring accurate measurement of effective breathing.
How Do You Calculate Alveolar Ventilation Rate?
Calculate alveolar ventilation by subtracting dead space volume from tidal volume, then multiply by respiratory rate. The formula is: (Tidal Volume – Dead Space) × Respiratory Rate.
Why Is Alveolar Ventilation Important For Health?
Alveolar ventilation determines oxygen supply to blood and carbon dioxide removal. Proper levels maintain blood pH and support cellular function, crucial for overall respiratory health.
What Is The Difference Between Tidal Volume And Alveolar Ventilation?
Tidal volume is the total air inhaled or exhaled per breath. Alveolar ventilation is the portion of that air reaching alveoli for gas exchange, excluding dead space.
Conclusion
Calculating alveolar ventilation helps understand how well your lungs work. It shows the amount of fresh air reaching the lungs for gas exchange. Knowing this can guide better breathing techniques and health decisions. Always remember to subtract dead space volume from total ventilation.
This simple step gives you the true measure of effective breathing. Keep practicing these calculations to improve your lung awareness. Clear, easy steps make the process less confusing. Understanding alveolar ventilation supports healthier living and better oxygen supply.