Have you ever wondered how ventilators help patients breathe when their lungs can’t do the job alone? One key setting you might hear about is called “AC Mode.”
Understanding what AC Mode in a ventilator means can be crucial, especially if you or a loved one is using one. This mode plays a vital role in supporting breathing, but it’s often surrounded by confusing medical jargon. You’ll discover exactly what AC Mode is, how it works, and why it matters for your health or the care of someone you care about.
Keep reading to unlock clear, simple answers that put you in control of your knowledge.
Basics Of Ac Mode
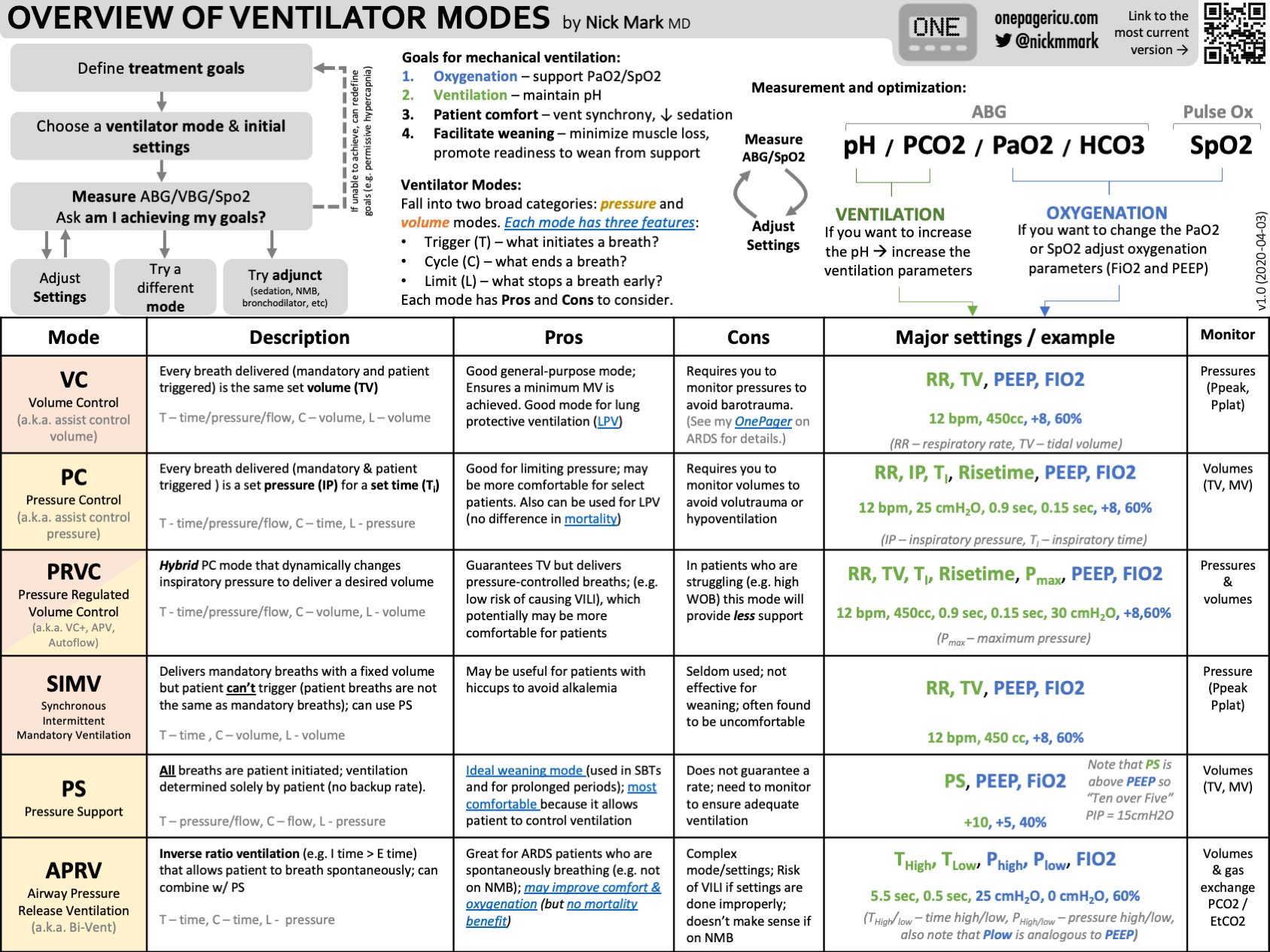
Understanding the basics of AC Mode helps in grasping its role in ventilators. AC Mode stands for Assist-Control Mode, a common setting in mechanical ventilation. It supports patients who cannot breathe well on their own. This mode provides a set number of breaths with a fixed volume or pressure. It ensures the patient receives consistent breathing support.
How Ac Mode Works
AC Mode delivers breaths in two ways. First, it gives mandatory breaths at a set rate. Second, it assists any extra breaths the patient tries to take. The ventilator senses the patient’s effort and helps by providing full support. This keeps the breathing steady and reduces work for the lungs. The machine controls the volume or pressure of each breath.
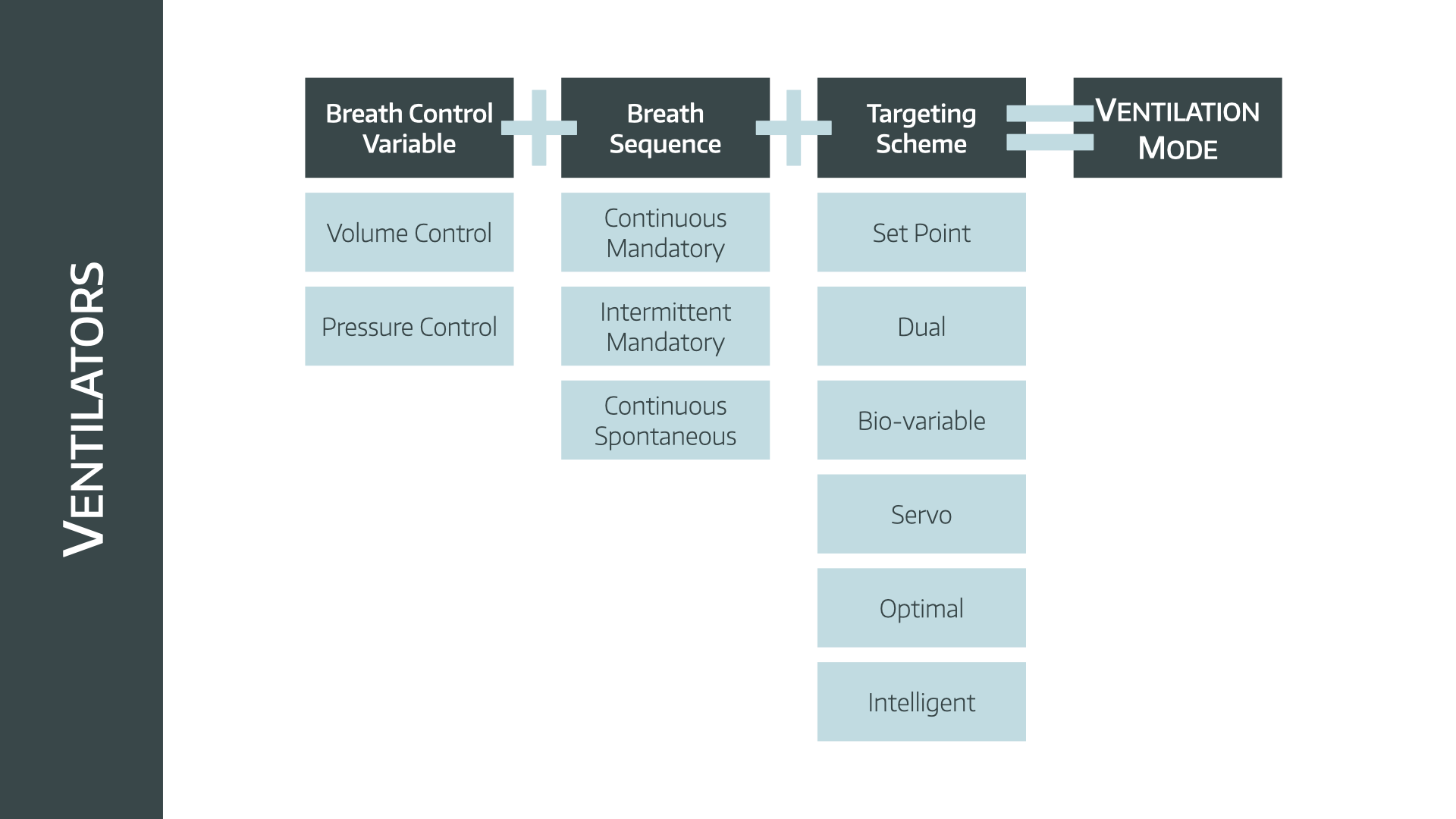
Types Of Ac Mode
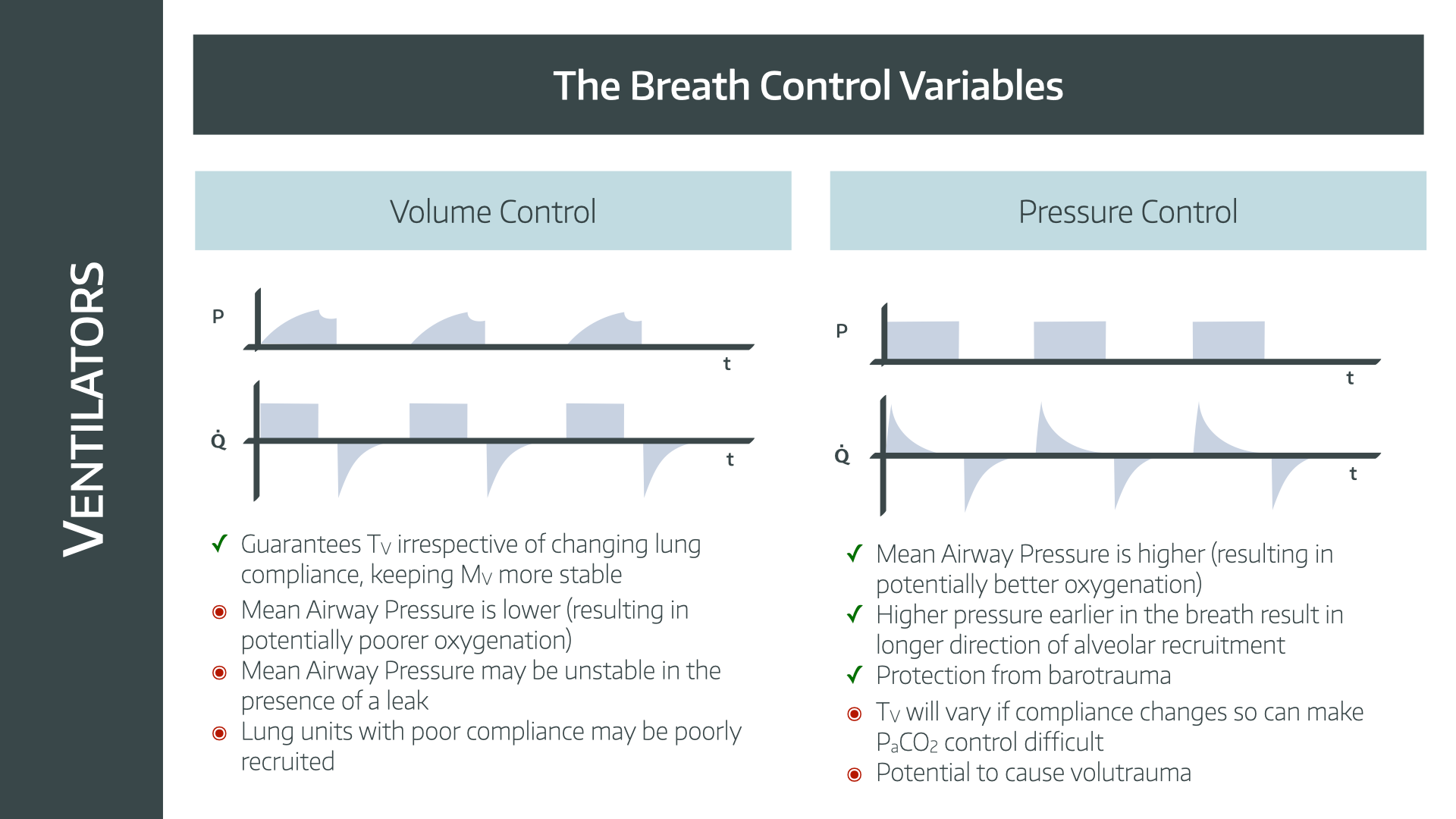
- Volume-Controlled AC:The ventilator delivers a fixed volume of air per breath.
- Pressure-Controlled AC:The ventilator maintains a set pressure during each breath.
Both types ensure the patient gets enough air. The choice depends on the patient’s condition and doctor’s decision.
When Ac Mode Is Used
AC Mode suits patients who need full breathing support. It is common in cases of respiratory failure or during surgery. Patients unable to breathe deeply or fast enough benefit from this mode. It helps keep oxygen levels stable. The mode also aids in rest and recovery.
Benefits Of Ac Mode
AC mode, or Assist-Control mode, in ventilators offers several key benefits. It helps patients breathe more easily by providing timely support. This mode adjusts to the patient’s efforts, making breathing smoother and more effective. Understanding the benefits can help caregivers and patients appreciate its value during respiratory care.
Improved Patient Comfort
AC mode delivers breaths in sync with the patient’s own breathing attempts. This coordination reduces discomfort and avoids breath mismatch. Patients feel less strain and more natural breathing support. The ventilator adapts to each breath, making the experience gentler and less stressful.
Enhanced Respiratory Support
The ventilator ensures a set minimum number of breaths per minute. It also supports extra breaths triggered by the patient. This dual function prevents low oxygen levels and carbon dioxide buildup. The steady support helps maintain healthy lung function and gas exchange.
Reduced Work Of Breathing
AC mode lowers the effort needed to breathe. The ventilator assists with every breath, easing the load on respiratory muscles. Patients conserve energy, which aids recovery and comfort. Less breathing effort means reduced fatigue and better overall health.
Settings And Adjustments
Settings and adjustments in AC mode are vital for patient comfort and safety. These controls help tailor the ventilation to match the patient’s lung needs. Proper tuning prevents lung injury and ensures efficient breathing support.
Each setting has a specific role. Changing one setting affects others, so care is needed. Healthcare providers monitor the patient’s response and adjust accordingly.
Tidal Volume Control
Tidal volume is the amount of air delivered with each breath. It usually ranges from 6 to 8 ml per kilogram of the patient’s ideal body weight. Setting the right tidal volume prevents lung overdistension or collapse.
The ventilator keeps tidal volume constant in AC mode. This ensures the patient gets enough air even if their effort varies. Adjust tidal volume based on blood gas results and lung condition.
Respiratory Rate Settings
Respiratory rate is the number of breaths per minute set on the ventilator. It works with tidal volume to control minute ventilation. Too high a rate can cause breath stacking and discomfort.
The rate can be adjusted to match the patient’s natural breathing or to provide full support. Monitoring oxygen and carbon dioxide levels helps fine-tune the rate.
Pressure And Flow Adjustments
Pressure settings control how much force the ventilator uses to deliver air. Flow rate determines how fast the air enters the lungs. Both affect patient comfort and ventilation efficiency.
Adjust pressure limits to avoid lung injury from excessive force. Flow rates can be set to match the patient’s inhalation effort, making breaths feel more natural.
Credit: www.anaestheasier.com
Clinical Applications
The clinical applications of AC (Assist-Control) mode in ventilators are essential to understand for anyone involved in respiratory care. This mode supports patients who cannot maintain adequate breathing on their own by delivering a set number of breaths while allowing them to initiate additional breaths. Knowing where and how AC mode fits into patient care can help you make better decisions for treatment and patient comfort.
Use In Acute Respiratory Failure
AC mode is often the first choice for patients with acute respiratory failure. It ensures a minimum number of breaths per minute, guaranteeing adequate oxygen delivery and carbon dioxide removal. Have you noticed how patients sometimes tire quickly? AC mode helps reduce their work of breathing by providing full support.
In cases like severe pneumonia or acute respiratory distress syndrome (ARDS), AC mode keeps the lungs ventilated even when the patient’s own effort is weak or absent. This can be lifesaving while other treatments take effect.
Role In Anesthesia
During surgery, AC mode supports patients under general anesthesia by maintaining steady ventilation without requiring patient effort. This keeps oxygen levels stable and carbon dioxide low, which are critical for safe anesthesia.
It also allows anesthesiologists to control the breathing rate and volume precisely, adapting to surgical needs. Have you ever wondered how breathing is managed when a patient is completely unconscious? AC mode answers that question effectively.
Application In Icu Patients
In the ICU, many patients depend on ventilators for extended periods. AC mode is valuable because it offers consistent support yet allows patients to trigger extra breaths, promoting comfort and synchrony with the machine.
This mode can be adjusted as patients recover, gradually reducing support to encourage spontaneous breathing. If you care for ICU patients, observing how they respond to AC mode can guide you in tailoring ventilator settings for the best recovery outcomes.
Potential Risks And Limitations
Ac Mode in ventilators supports breathing by delivering set breaths at fixed volumes or pressures. Despite its benefits, this mode carries potential risks and limitations. Understanding these drawbacks helps in making safer clinical decisions and improving patient care.
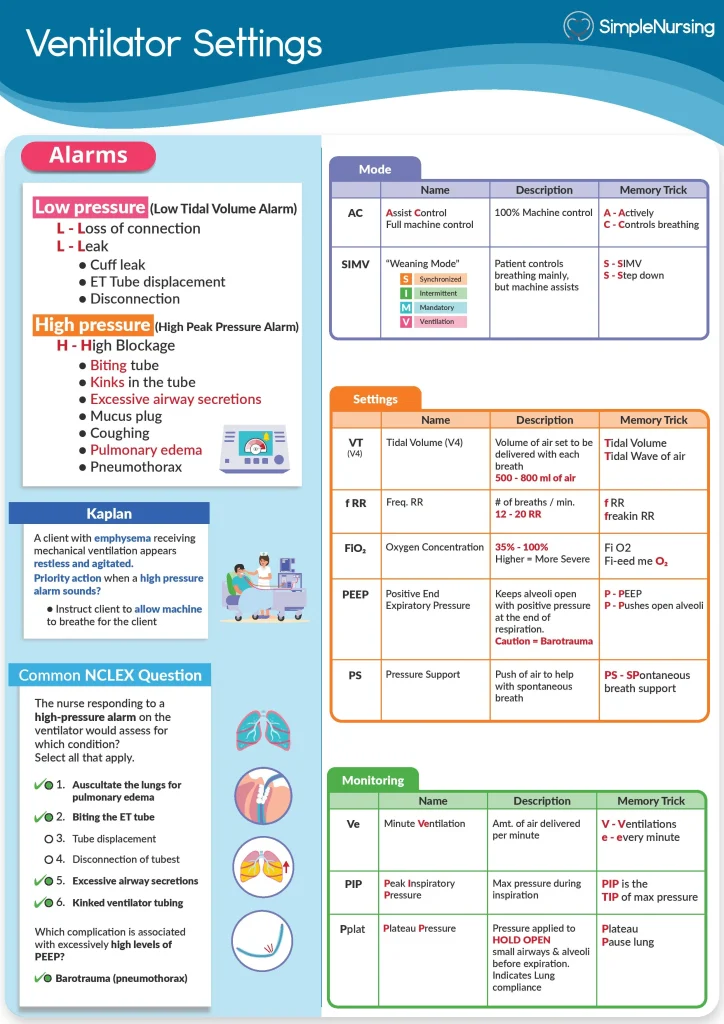
Risk Of Hyperventilation
In Ac Mode, the ventilator delivers breaths regardless of patient effort. This can cause breathing faster than needed. Excessive ventilation lowers carbon dioxide levels in the blood. Low carbon dioxide may lead to dizziness, muscle cramps, or fainting. Careful monitoring is essential to avoid these complications.
Patient-ventilator Asynchrony
This occurs when the ventilator’s timing does not match the patient’s breathing. It can cause discomfort and increased work of breathing. Signs include coughing, fighting the ventilator, or irregular breathing patterns. Adjusting settings or switching modes may be necessary to improve comfort and support.
Contraindications
Ac Mode is not suitable for every patient. Those with irregular breathing patterns or weak respiratory muscles may struggle. Patients who cannot tolerate fixed breath volumes or pressures require alternative ventilation modes. Always assess patient condition before choosing this mode.
Credit: www.anaestheasier.com
Comparisons With Other Ventilator Modes
Ac Mode in ventilators provides continuous support, offering a steady flow of breaths. It is often compared to other modes like SIMV and CPAP, which allow for more spontaneous breathing.
Understanding the differences between ventilator modes is crucial for healthcare professionals and caregivers alike. Each mode offers unique features suited to various patient needs. Let’s dive into how AC Mode stacks up against other popular ventilator settings.Ac Mode Vs Simv
AC (Assist-Control) Mode provides full ventilatory support, automatically delivering breaths at set intervals. This can be beneficial for patients needing consistent assistance. However, some patients may become too dependent on the machine. In contrast, SIMV (Synchronized Intermittent Mandatory Ventilation) Mode allows patients to breathe spontaneously between mandatory breaths. This can help wean patients off the ventilator more smoothly. SIMV offers a balance of support and independence, promoting gradual respiratory strength.Ac Mode Vs Cpap
AC Mode is ideal for patients who require consistent breathing assistance. It ensures complete control over the breathing process. But, it might not be the best choice for patients who can breathe independently. CPAP (Continuous Positive Airway Pressure), on the other hand, is often used for those with sleep apnea. It maintains airway patency and supports spontaneous breathing without delivering mandatory breaths. CPAP can be a more comfortable option for patients who need less invasive support.Ac Mode Vs Pressure Support
AC Mode provides a fixed breath pattern, beneficial for patients unable to initiate breaths. It helps maintain adequate ventilation even when the patient is passive. Pressure Support Mode encourages patients to initiate breaths while providing additional pressure to ease breathing. This mode is excellent for those ready to transition to independent breathing. It promotes active participation in the breathing process, supporting respiratory muscle strengthening. How do you decide which mode to use? Consider the patient’s current condition and the level of support they need. Each mode has its place in treatment, and understanding these differences can enhance patient outcomes.Tips For Optimizing Ac Mode
Optimizing AC mode in a ventilator ensures better support and comfort for patients. Careful management of settings and patient monitoring helps avoid complications. Small adjustments can make a big difference in breathing support and overall outcomes.
Monitoring Patient Response
Check the patient’s breathing patterns often. Watch for signs of distress or discomfort. Monitor oxygen levels and carbon dioxide removal. Use alarms and alerts to catch any problems early. Keep notes on changes to adjust settings promptly.
Adjusting Settings For Comfort
Start with gentle pressure and volume settings. Increase support only as needed. Adjust the trigger sensitivity to match patient effort. Avoid causing too much pressure, which can harm lung tissue. Tailor settings to the patient’s size and lung condition.
Avoiding Common Mistakes
- Do not set pressure too high; it may cause lung injury.
- Avoid ignoring patient signs of discomfort or pain.
- Do not forget to check ventilator alarms regularly.
- Never leave settings unchanged for long without review.
- Ensure clear communication among healthcare staff about changes.
Credit: www.anaestheasier.com
Frequently Asked Questions
What Does Ac Mode Mean In A Ventilator?
AC mode stands for Assist-Control mode. It delivers a set number of breaths at a fixed volume or pressure. It assists patients by triggering additional breaths when needed, ensuring adequate ventilation.
How Does Ac Mode Benefit Ventilated Patients?
AC mode provides consistent breathing support. It helps patients who cannot breathe fully on their own. The ventilator assists every breath, improving oxygen delivery and reducing work of breathing.
When Is Ac Mode Used In Ventilation Therapy?
AC mode is used for patients with weak respiratory muscles or respiratory failure. It ensures full ventilatory support, especially during surgery or critical illness when spontaneous breathing is insufficient.
Can Patients Trigger Breaths In Ac Mode?
Yes, patients can trigger additional breaths above the set rate. The ventilator senses their effort and delivers full support, making breathing easier and more comfortable.
Conclusion
AC mode in a ventilator helps support breathing by controlling breaths. It gives a set number of breaths with a fixed volume or pressure. This mode suits patients who need full or partial breathing support. Understanding AC mode helps caregivers make better decisions.
It ensures patients receive proper breathing assistance. Knowing its function improves patient care and safety. Always follow medical advice when using ventilators. Clear knowledge makes a difference in treatment outcomes.